125 years of care: History at a glance
We started by scraping together $752
Salem Health’s journey began in 1896 with about $752 to turn the former Oregon School for the Blind into a five-bed hospital. It was on 12th Street near the current Willamette Heritage Center.
Our first patient was Fred Demeter, 65-year-old sewing machine salesman. He paid $5 for hip surgery and $1 a day to recover for 28 days.
The rest is history, with competition, mergers, floods, pandemics, wars, depressions, the creation of private health insurance, Medicare, vaccines, vitamins — and technology. You name it, Salem Health has tackled it and remained focused on its mission
— to improve the health and well-being of the people and community we serve.
Chapter one: Early history – two hospitals are born
Our first hospital was opened in the former Oregon State School for the Blind in 1896. In late 1895, Mrs. J.J. Murphy raised $752 with help from local farmers, grocers, shop owners to renovate the building near the Thomas Kay Woolen Mill. A medical student was house physician and three nurses ran the hospital.
In 1916 the hospital’s first competitor, the Deaconess Home and Hospital, was founded by Franz Wedel and four Mennonite deaconesses; Sisters Marie Wedel, Martha Wedel, Marie Duerksen and Anna Duerksen. It was in the former Capitol Hotel, an ornate three-story building. Patients were carried up and down staircases. A stay in a hospital room was $2.50 a day.
Key dates and events:
1900 — Salem population at 4,258
1896 — Salem Hospital established
1899 — Hospital moves to former Glen Oak Orphans Home
1903 — EKG is invented
1906 — First female doctor in Salem, Mary Purvine
1912 — Vitamins are discovered
1916 — Deaconess Home and Hospital started by Frank and Helene Wedel
1919 — Salem Hospital threatened with closing during flu pandemic

Deaconess Hospital circa 1918
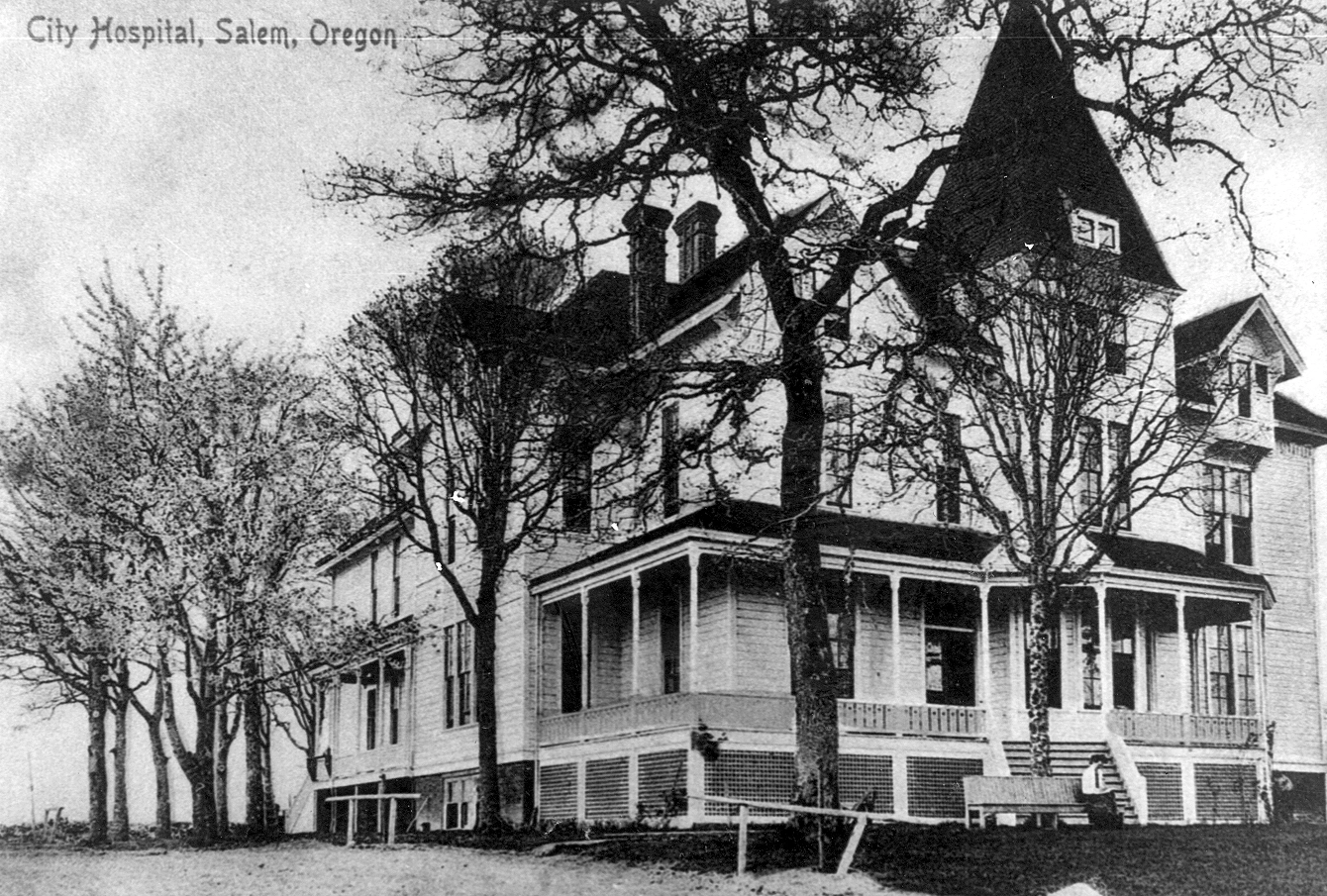
Salem City Hospital in 1896

Nurses attend to babies in the Salem Hospital nursery of the 1950s
Chapter two: Facing financial hardship; community takes over
By 1931, Deaconess hospital’s founder Franz Wedel was replaced by his son Frank; Frank’s son Irwin took over in 1948. Much was done through charity, but the hospital was in need of cash, so Pioneer Trust Bank loaned the hospital $50,000 on the condition that the hospital would be taken over by the community.
So Deaconess Hospital became Salem Memorial Hospital. Around the same time, the original Salem Hospital changed its name to Salem General.
Auxiliaries were formed — yes, they were called “women's auxiliaries” — for both hospitals in the 20s and 30s to strengthen community support. Six percent of Americans had health insurance in 1939 – but by 1950, about 50 percent did, so hospitals needed help!
As technology grew, we added equipment and staff, including the first board-certified surgeon in 1946. More advancements arose from WWII and more patients arrived with the baby boom, and so did the need to keep better track of them, so they began a medical records system.
The political climate fostered by local physicians seeing more patients and medical advancements fed movement to modernize even faster, laying the foundation for major growth during the 1950s and 60s.
Key dates and events
1920 — Salem population 17,679
1924 — First X-ray machine arrives in Salem
1925 — First lab technician hired
1927 — Changed name to Salem General Hospital
1928 — Women’s
Auxiliary formed
1939 — Women’s Auxiliary formed at Salem Deaconess Hospital
1940 — Salem population 32,398
1946 — First surgeon, Dr. Robert Wulf, arrives
1947 — Salem Deaconess Hospital changes name to Salem Memorial
1952 — Polio vaccine invented
Chapter three: Hospitals merge; bequests, specialties arrive
We kept pace with rapid changes during the ‘60s with improved lab and pharmacy services, the first surgical ICU, the start of computers and hiring social workers. Salem Memorial was the first hospital in the US to receive EKG data by phone!
Both hospitals added buildings for growth, but Memorial was more financially sound and grew faster, building a 42-bed addition in 1953. (175 beds were added in one 15-year period). Seeing these trends, including the need to coordinate modernization, physicians and civic leaders began to push for a single regional hospital. So in 1969, Salem General and Salem Memorial became Salem Hospital.
The plan worked. In the first 10 years, this union saved $27 million by eliminating duplicate equipment purchases. The campus was busy with more remodeling and additions during the 1980s and ‘90s.
But our community-minded board knew other needs were emerging, so they added specialized services, such as psychiatric medicine and urgent care.
Key dates and events
1960 — Salem population 49,122
1964 — Evacuation during massive flood
1968 — Hospital Foundation established
1969 — Salem General and Salem Memorial merge
1974 — Alice Yoshikai becomes first female board member
1978 — First CT scanner arrives
1980 — Salem population 89,091
1986 — First $1 million bequest from Lamport estate
1988 — Psychiatric
Medicine Center begins; first MRI appears
1989 — First open heart surgery; 24-bed rehabilitation unit opens
1995 — Urgent care opens

Salem Hospital is evacuated during the 1964 Christmas flood
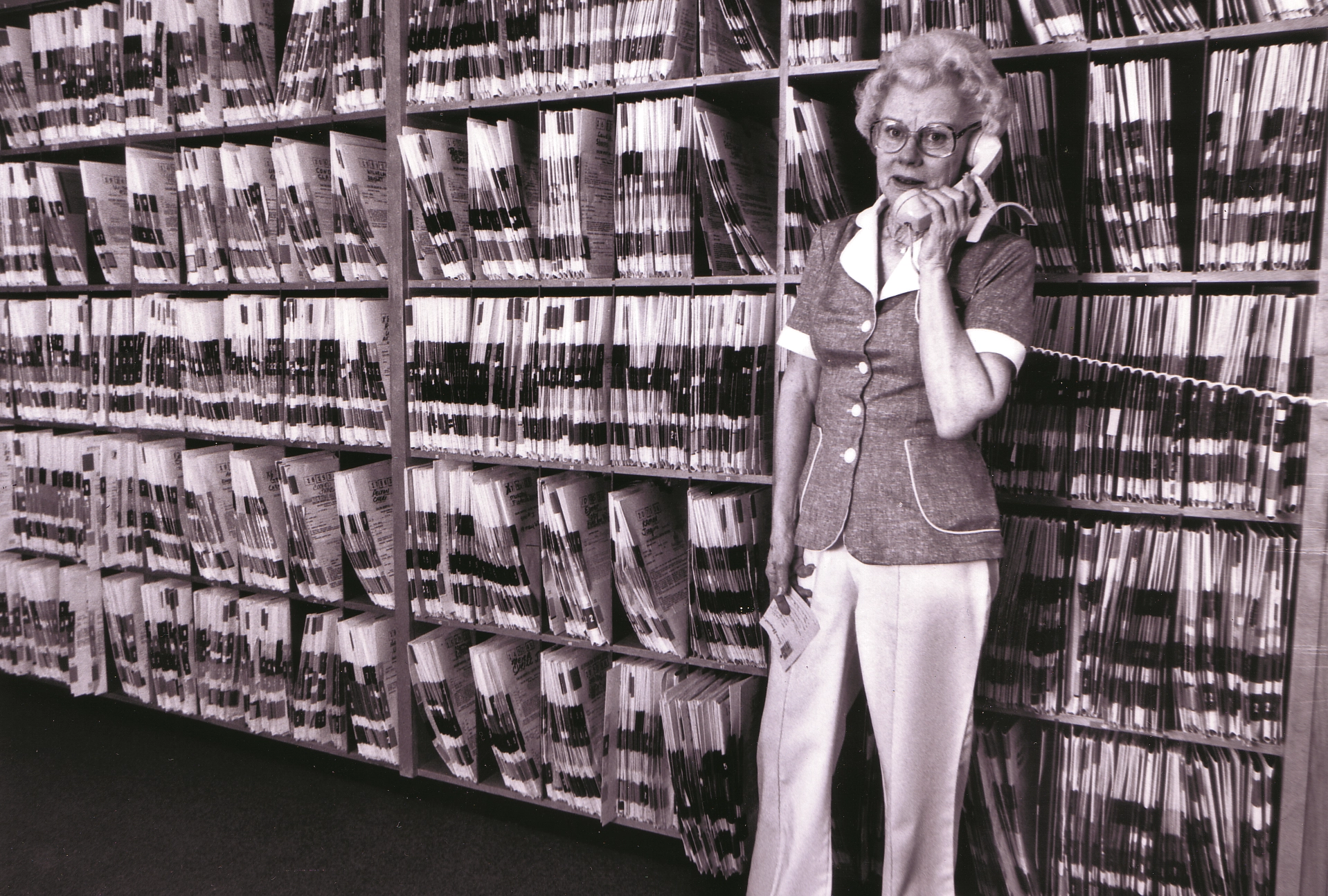
Medical records and X-rays took up a lot of space in the 1970s

Building B in 1994, viewed from the east

Salem Hospital's Relay For Life team in 1999

West Valley Hospital officially joined the Salem Health family in 1999.

Building A's critical care tower (home of the Salem Hospital emergency room) opened in 2009.
Chapter four: Thinking ahead pays off as service, reputation grows
Salem Health has always put its community’s health care first by thinking ahead. By the end of last century, we were attracting the best — physicians, staff, equipment, and major additions such as the Family Birth Center.
Awards started rolling in (and continue each year), putting us on the map as a top hospital, not only regionally, but nationally.
With surgery techniques becoming less invasive (before 1990, removing a gall bladder was major surgery; now it’s day-surgery) we built the Outpatient Surgery Center (now Building C) in 2000. Leaders were also thinking ahead as our population grew, by purchasing land — and another hospital in Dallas.
At the close of the 20th century, we were on our way to reaching two major goals: providing clinical quality second to none, and enhancing programs, technologies, facilities and community partnerships. We had a strong fundraising Foundation, and an army of volunteers.
We realized the need for preventive health care and meeting the needs of an increasingly diverse population. And, an aging one, with more chronic, critical-care needs. So we built what was to be a crown jewel — the Building A tower.
And we invested in preventive care and wellness through the Community Health Education Center to provide free health information, support groups, inexpensive (or free) classes — even a “wellness kitchen” to teach nutrition.
Salem Hospital joined the revolution of electronic medical records (EMR) by purchasing Epic in 2006, placing it in the top 5% of Oregon’s hospitals using EMR. Epic put health data in our hands in seconds. Then in 2010, providers began entering their medical orders electronically through CPOM (computerized provider order management), eliminating hand-written orders.
Key dates and events:
2000 — Salem population 136,924
2001 — Center for Outpatient Medicine (Building C) opens
2002 — Valley Community Hospital bought, becomes West Valley Hospital
2003 — Family Birth Center (Building D) opens
2003 — New Emergency Room opens as part of Building B
2005 — Hospitalists began 24-hour physician coverage for inpatients
2007 — We earn the first of six prestigious Beacon Awards given in next few years for critical care
2009 — Critical Care Tower (Building A) opens with helipad.
Chapter five: The mission continues through a pandemic
The most recent 10 years bring us to the present, with exponential growth, one major failure but accomplishments that kept us moving forward.
We triumphed with more new facilities, clinical accomplishments and collaboration, including a ground-breaking compact formed between hospital administration and medical staff. Its only focus: To improve patient care.
About that failure ... It’s important to acknowledge things that don’t work out, because it’s part of our history – and in being honest. Facing market challenges, we began a partnership with Oregon Health & Science University in 2015. Although the effort didn’t pan out, this bold venture showed we had the courage to try. The partnership ended in 2017.
Community outreach increased, enhanced by our largest public outreach campaign, “You Matter” that continues to this day. Then in the wake of the racial violence surfacing boldly in 2020, a significant, board-driven focus emerged to increase diversity and inclusion awareness.
No patient harm is acceptable to us became our mantra and is included in almost every communication with staff – including on whiteboards in offices and staff rooms. The Peer Support Program formed in 2018 validated the trauma our own staff face “on the front line,” showing a major investment in staff and provider mental health.
On the eve of the Covid-19 pandemic, we broke ground on the latest expansion in January 2019. By March, thanks to an outstanding “Incident Command” system, we were poised to tackle the virus with surge plans and staff in place – which changed daily to adapt to new rules and emerging information.
While our clinic side geared up, our online presence exploded with resources, reaching thousands of worried and panicked people with daily direction to navigate the pandemic and subsequent vaccination efforts.
Humming loudly in the background, campus expansion continued all year – on schedule to open in 2022. We’re ready for the next 125 years. The culture of Salem Health has always been to adapt and respond, to stay ahead of the game.
Just like they did with $752 to turn a school into a hospital in 1896.
Key dates and events to the present:
2010 — Salem population 154,637
2010 — Community Health Education Center opens, Salem Hospital earned Magnet Designation
2011 — Inpatient rehab moves from Center St. location to new Build. B unit
2011 — Salem Health, medical providers form “Common Ground Compact” to improve
care
2013 — Emergency Dept. designated Level II Trauma Center
2014 — Outpatient Rehabilitation Center opens (Building M)
2015 — Salem Health, OHSU form OHSU Partners (dissolves in 2017)
2015 — Cheryl
Wolfe becomes first female CEO: Magnet Designation status renewed
2017 — Let’s All Play Place inclusive playground opens
2018 — Salem Hospital earns Gold Beacon for intensive care
2020 — Salem population 177,803
2020 — Construction begins on 7-story tower next to Building A to serve an aging population, providing 150 more beds, to open in 2022
2020 — Covid-19 pandemic and lockdown begins

Today, Salem Health is more active than ever in community outreach, including Salem's holiday toy drive!

When the vaccine became available, Salem Health jumped into action, opening the state's first mass vaccination clinic for COVID-19.

Construction began on a new patient care tower at the beginning of 2020. The building is expected to be completed in 2022.